Morgan & Masterson Consulting
Selection of Clinical Biomaterials
Selection of Clinical Biomaterials
When I entered this profession, the materials used in medical devices were not subject to the rigors of standard specifications or regulatory-prescribed safety testing, nor were there records of ‘acceptable materials’; it was, literally, a cottage industry, with many devices incorporating well- known fabrics, alloys, gels, fibers and plastics that had traditional household or industrial uses. There were no academic centers providing knowledge or experience about suitable materials – in 1968, my laboratory in Liverpool was one of the first in Europe to focus on this subject.
But slowly things changed – they had to. Steels were corroding in the body, metallic plates and rods became deformed because anatomy and elasticity could not be matched, plastics quickly wore out, elastomers started to crumble and gels would migrate, and many materials placed within circulating blood rapidly thrombosed. So, biomaterials laboratories were established, academic journals on biomaterials science found their way to library bookshelves and biomaterials societies were formed, in the USA and then in Europe.
Over the years, the number of clinically-applied biomaterials increased, although few were specifically designed for use within the body. Although some of the most unsuitable of these materials were eliminated from consideration because of demonstrably poor performance, catalogues of biomaterials kept getting larger, especially within the realm of polymers, where variations on a simple structure, through copolymers, blends, composites, surface treatments and so on, expanded the repertoire enormously. This scenario has been tempered somewhat in recent years as standard specifications introduced by bodies such as the International Standards Organization (ISO) and the American Society for Testing and Materials (ASTM) defined precise compositions and performance specifications, and as regulatory bodies such as the Food and Drugs Administration (FDA) demanded compliance with these characteristics.
The selection of materials for a specific application, however, involves a great deal more than plugging the required performance requirements into a searchable database and coming up with the ideal match; there are no algorithms here since clinical performance is influenced by a multitude of factors, and since a very wide spectrum of material characteristics join together, sometimes antagonistically, sometimes synergistically, sometimes totally independently, to determine outcomes.
This is where the knowledge and experience of a consultant comes in. Such a consultant may be retained by a materials company that is developing and supplying new products to the industry and needs to know how the properties of candidate materials can be refined and targeted to device applications. Alternatively, the consultant may be retained by a medical device manufacturer that has defined the ‘user needs’ for a new product and has to select the most appropriate material(s) to satisfy those needs.
Consulting for Biomaterials Companies
The biomaterials supply chain incorporates several different types of companies, ranging from major multinationals with either chemicals, materials or pharmaceuticals expertise and capacity, to small specialist groups, either university-based spin-offs or discrete start-ups derived from the major conglomerates. Whilst the attractiveness of high added value within the healthcare sector, often with very limited development costs, led to the rapid involvement of these major players within the medical device sector, including Dow Chemicals, 3M, Pfizer, Bristol Myers Squibb, and DuPont, the realization that this could attract profound litigation if things went wrong, forced many of them to rethink and find other ways to be involved. The field is now dominated by the smaller companies that are structured to be legally and financially distant from these major companies. In this form, such companies often do not have requisite skills in-house and rely extensively on outside consultants. Some examples are given here briefly:
Polyetheretherketone (PEEK) and other thermoplastic polymers
Degradable polymers
Surface coatings
Bioactive ceramics

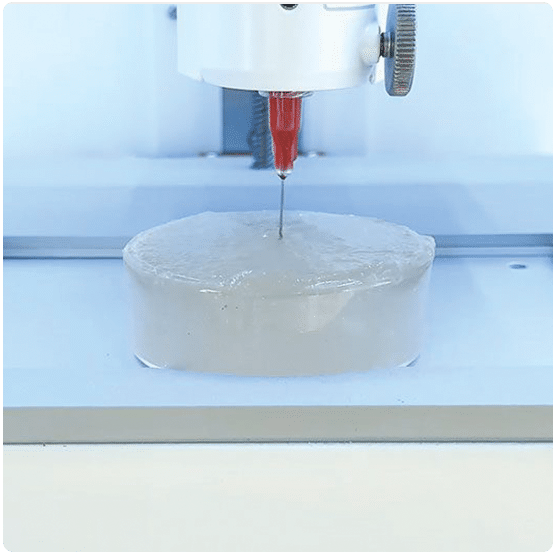
Bioprinting gels and inks
Consulting for Medical Device Companies
Since, as noted earlier, there are now many internationally-recognized standards for biomaterials compositions and functional performance, it might seem to be a straightforward task to consider the details of a device ‘user needs’ file and select the most suitable materials from those standard lists. This is not necessarily the case. Consider the situation, for example, of a drug-eluting coronary artery stent. This, indeed, does look straightforward as the product consists only of a metallic framework and a thin, drug-containing, polymeric coating on that framework. Naturally, in the product development process, design and materials characteristics are considered together, but the overall characteristics that determine clinical outcomes will include elasticity (and possibility superelasticity), fatigue and creep, metallic biocompatibility, polymer stability or degradability, polymer-drug compatibility, drug diffusion, polymer biocompatibility, drug pharmacokinetics and device thrombogenicity. These considerations require a wide array of expertise and experience attributes.
Alloys for orthopedic devices

Tissue engineering scaffolds
Anti-bacterial silver devices
Morgan & Masterson Consulting
We offer global, high-level consulting for scientific and infrastructure aspects of cutting-edge medical technologies.
Our Expertise
Work with Us
We are commited to making a global impact and providing cost-effective solutions.