The Need for Innovative Technologies
Approximately three decades ago, conditions such as hypertension and atherosclerotic heart diseases were rare in Africa, and communicable diseases were the major causes of death. However, over this same period, non-communicable diseases have shown a remarkable rise. Cardiovascular disease now surpasses HIV/AIDS, malaria and other enteric infections in the top causes of death, rising from the 6th to the 2nd leading cause of death in sub-Saharan Africa between 1990 and 2019. The underlying drivers have been marked increases in major risk factors, such as hypertension and diabetes, off-setting the substantial health gains made with communicable diseases. The underlying epidemiological shift has been heavily influenced by urbanization, reflected in the nutritional and activity transitions.
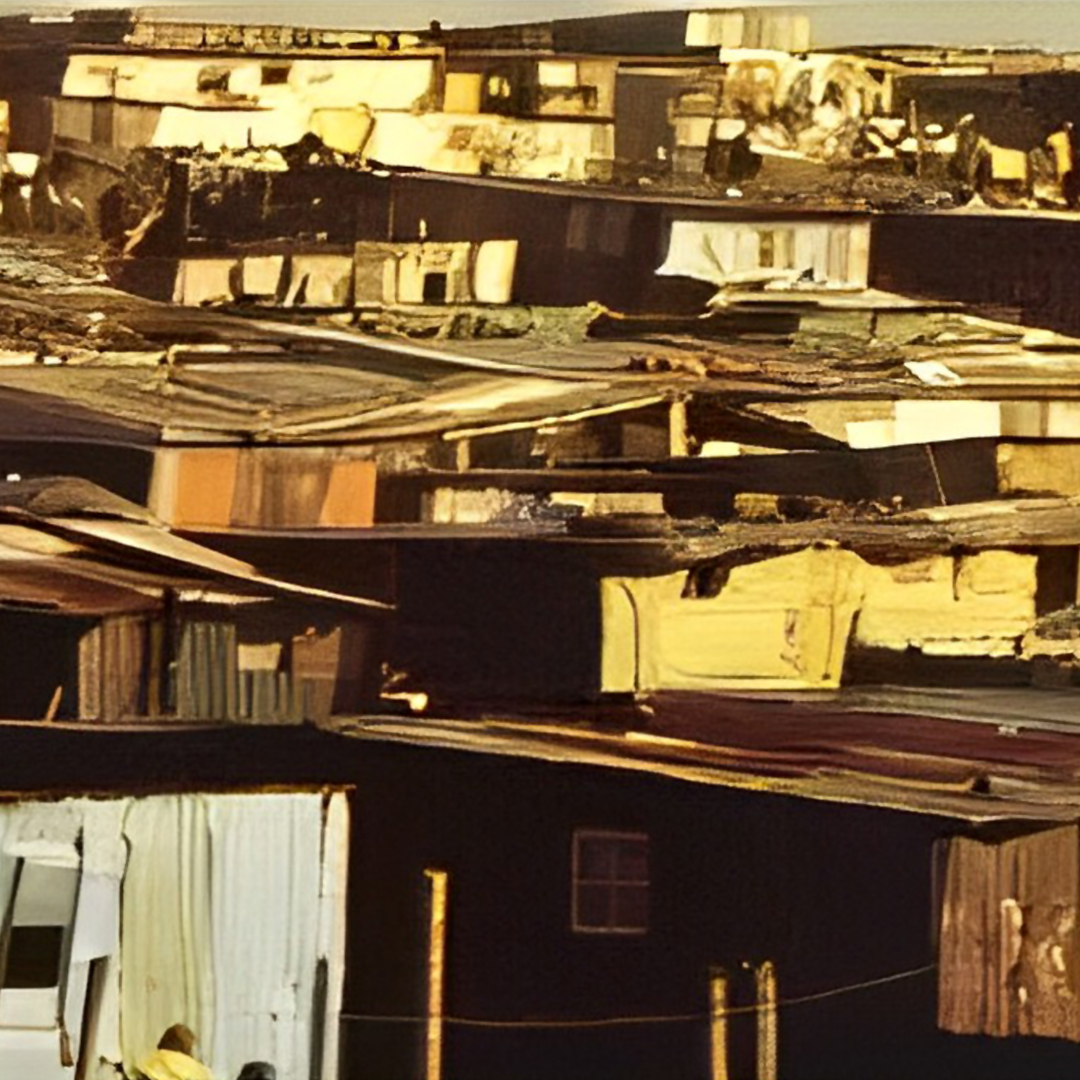
Rheumatic heart disease (RHD) is one of the most significant cardiovascular conditions in sub-Saharan Africa, especially seen in the densely-crowded townships.
It results from recurrent episodes of acute rheumatic fever following a streptococcal throat infection, thought to be an autoimmune-mediated response to interactions between the individual and certain components of the bacterial cell wall protein.
RHD is Estimated to Affect 40 Million People Worldwide
RHD is estimated to affect forty million people worldwide, the majority of whom are children and young adults in sub-Saharan Africa: around 400,000 die from RHD annually, with an average age at death in some regions as low as 28 years. RHD continues to take a heavy toll on many people in lower‐income countries, making it among the most neglected diseases relative to its burden worldwide. Until there is an effective vaccine for RHD prevention, the WHO suggests following a preventive approach associated with improved socioeconomic status of populations at risk, primary prevention, including treating patients with strep throat, secondary prevention of antibiotic prophylaxis among patients with previous rheumatic fever, and tertiary procedures, including medical/surgical treatment of symptomatic RHD. The evidence suggests that every seventh to tenth patient with RHD would need life- saving heart valve surgery.
It was the latter approach, concerning innovative surgical treatments for RHD patients, which stimulated the formation of the company Strait Access Technologies (SAT) in Cape Town, South Africa more than a decade ago. Several critical features of the disease and of the individuals that it affects, were the drivers of the vision of the two founders of the company, myself and Professor Zilla, then the Chris Barnard Professor of Cardiothoracic Surgery at the University of Cape Town. They were soon joined by Dr Deon Bezuidenhout (also of UCT). Their vision was that a combination of advanced principles of medical engineering and cardiovascular medicine could make a significant contribution to the preservation of quality of life for young people in many parts of Africa, and, indeed, in many other parts of the world.
Important Factors for SAT's Vision to Improve Quality of Life for Children and Young Adults in Sub-Saharan Africa with RDH
The reality of limited access
The principal clinical manifestations of RHD are seen with the valves of the heart. Progressive valvular disease commonly develops after a few episodes of acute rheumatic fever. Around 70% of children with rheumatic fever develop chronic valvular disease over the following decade or so, 15% of whom progress to severe disease states. According to the Cape Town Declaration on Access to Cardiac Surgery in the Developing World, the only effective treatment for RHD is open heart surgery; however, the availability of cardiac surgery facilities capable of performing the necessary surgical procedures for RHD patients in low-to-middle income countries is often very low, so that the people most at need of such surgery are unlikely to have the necessary access. Any new technology for treating RHD could not therefore rely on conventional cardiac surgical techniques.
TAVR,
The first open heart surgery procedures, using cardiopulmonary bypass, date back to the 1950’s, and heart valve replacements were initiated in the early 1960s. Successful as these were, they were largely confined to high-income countries; however, as individual longevity increased so did the number of patients in need of them, but often with co- morbidities that affected the ability to survive the bypass procedure. It became obvious that new approaches were needed and by the turn of the century, the minimally invasive techniques for accessing the aortic valve of the heart by means of a catheter threaded along a blood vessel, most commonly along the femoral artery starting in the groin area, was introduced; this technique was referred to as Transcatheter Aortic Valve Replacement (TAVR). As TAVR became more effective, in these highly resourced countries, it was apparent that they would have little impact in poorer, socio-economically deprived regions; such a major transformation would require simpler transcatheter procedures that could deploy valves cost-effectively without sophisticated healthcare infrastructure. Any new technology for treating RHD in low-to-middle income regions could not, therefore, rely on the then conventional TAVR technology.
The clinic-pathological barrier
There was one more highly significant clinic-pathological barrier to the use of the TAVR techniques for aortic valve conditions in those suffering from RHD. The majority of patients recommended for TAVR in high-income countries are elderly and exhibit aortic stenosis that involves a complex calcification process. The replacement valve can be anchored on the calcified tissue within the aortic annulus. However, in those with RHD, the pathology is not usually that of calcific stenosis, which restricts flow of blood through the valve, but of non-calcific regurgitation, which allows a significant degree of retrograde blood flow. Aortic valve regurgitation is a relative contraindication to TAVR because of the absence of calcification, which hinders valve anchoring and increases the risk of prosthesis embolization. Any new technology for treating non-calcific aortic regurgitation (the majority) could not, therefore, rely on the TAVR technology that had been developed for elderly aortic stenosis patients.
The reality of limited access
The principal clinical manifestations of RHD are seen with the valves of the heart. Progressive valvular disease commonly develops after a few episodes of acute rheumatic fever. Around 70% of children with rheumatic fever develop chronic valvular disease over the following decade or so, 15% of whom progress to severe disease states. According to the Cape Town Declaration on Access to Cardiac Surgery in the Developing World, the only effective treatment for RHD is open heart surgery; however, the availability of cardiac surgery facilities capable of performing the necessary surgical procedures for RHD patients in low-to-middle income countries is often very low, so that the people most at need of such surgery are unlikely to have the necessary access. Any new technology for treating RHD could not therefore rely on conventional cardiac surgical techniques.
TAVR,
The first open heart surgery procedures, using cardiopulmonary bypass, date back to the 1950’s, and heart valve replacements were initiated in the early 1960s. Successful as these were, they were largely confined to high-income countries; however, as individual longevity increased so did the number of patients in need of them, but often with co- morbidities that affected the ability to survive the bypass procedure. It became obvious that new approaches were needed and by the turn of the century, the minimally invasive techniques for accessing the aortic valve of the heart by means of a catheter threaded along a blood vessel, most commonly along the femoral artery starting in the groin area, was introduced; this technique was referred to as Transcatheter Aortic Valve Replacement (TAVR). As TAVR became more effective, in these highly resourced countries, it was apparent that they would have little impact in poorer, socio-economically deprived regions; such a major transformation would require simpler transcatheter procedures that could deploy valves cost-effectively without sophisticated healthcare infrastructure. Any new technology for treating RHD in low-to-middle income regions could not, therefore, rely on the then conventional TAVR technology.
The clinic-pathological barrier
There was one more highly significant clinic-pathological barrier to the use of the TAVR techniques for aortic valve conditions in those suffering from RHD. The majority of patients recommended for TAVR in high-income countries are elderly and exhibit aortic stenosis that involves a complex calcification process. The replacement valve can be anchored on the calcified tissue within the aortic annulus. However, in those with RHD, the pathology is not usually that of calcific stenosis, which restricts flow of blood through the valve, but of non-calcific regurgitation, which allows a significant degree of retrograde blood flow. Aortic valve regurgitation is a relative contraindication to TAVR because of the absence of calcification, which hinders valve anchoring and increases the risk of prosthesis embolization. Any new technology for treating non-calcific aortic regurgitation (the majority) could not, therefore, rely on the TAVR technology that had been developed for elderly aortic stenosis patients.
With these guiding principles in mind, the founders of SAT (later renamed SATH) recognized that several other important geo-political / socio-economic, clinical and technological factors had to be taken into account:
- The driving force for the creation of SATH, being based within Africa, was the absolute clinical need for RHD treatment on that continent, especially in Sub-Saharan countries. However, RHD is not confined to these regions; it is endemic in many other parts of the world, especially in low-income countries in East / South-East Asia and the Indian sub- continent, parts of South America and in Eastern Europe / former Soviet regions. In many of these counties, trends in urbanization and industrialization have led to transitions from low - income to middle - income status, so that although RHD is still highly prevalent, there is a greater economic environment to sustain innovative healthcare programs. Chief of these areas are the so-called BRICS countries (Brazil, Russia, India, China as well as South Africa). SATH has been mindful that successful commercialization of its products would eventually benefit from expansion of availability to these rapidly developing regions.
- RHD can affect all four valves of the heart, but especially on the left side, the mitral valve being affected as much as the aortic valve. Although SATH considered developing a technology platform that could address both aortic and mitral valve conditions, and indeed made some progress with mitral technology, it was decided that available resources did not allow these two developments to proceed in parallel, and most attention has been given to replacement of the aortic valve in RHD patients.
- The majority of commercially-available TAVR products are delivered transfemorally to replace the diseased native valve and consist of a metallic frame that supports leaflets made of animal tissue, hence the descriptor bioprosthetic TAVR. Although TAVR has many advantages, increasing experience has also revealed a number of risks and complications, especially associated with the delivery process. Annular rupture, inadvertent coronary artery occlusion, and the development of high-grade heart block with bradycardia are serious and sometimes life-threatening complications. A significant problem arises from the fact that with these stent-based devices, blood is still flowing through the aortic annulus during deployment, making the placement a difficult procedure. Many procedures are therefore performed with rapid ventricular pacing to allow the clinician a steadier implantation site. There are potential adverse consequences of this temporary pacing, and a technology that avoided such pacing would be significantly advantageous. A major technology platform designed and introduced by SATH is a non-occlusive, hollow-balloon catheter system that may be used without pacing.
- Two features of this balloon system concern the delivery route and the stent expansion mode. SATH determined that a transapical delivery route was best suited to this balloon system (in view of the primary aim of treating aortic regurgitation within the non- sophisticated conditions in low-to-middle income regions), and that, in common with the one global market-leader with TAVR, a balloon-expansion stent rather than a self- expanding shape memory alloy stent would be the preferred option. SATH’s technology, therefore, involves a balloon expansion system, delivered, in the first iteration, by the transapical route.
- Since traditional mechanical valves cannot be collapsed inside catheters, all of the TAVR systems developed to date have incorporated bioprosthetic leaflets. The first iteration of the SATH TAVR is similarly constructed from animal tissue, although the anti- calcification treatment of their bovine pericardium involves the proprietary procedure developed by the Zilla team in Cape Town.
- Notwithstanding the above comment, it has been acknowledged that bioprosthetic leaflets are subject to changes over time and recent evidence suggests that greater amounts of structural change may be seen in some TAVR devices than in surgical valves. A logical alternative would be to use degradation-resistant synthetic polymers in place of bioprosthetic tissue. At that time, no such polymer, and no such polymeric-based valve, existed. Because of the significant regulatory hurdles anticipated for a highly innovative valve that used, for the first time, a non-occlusive balloon expandable stent-based system, it was considered that adding a totally new polymeric valve would make regulatory approval that much more difficult. It was decided, therefore, to develop the bioprosthetic valve for first clinical use, and to work in parallel on a polymeric valve, with many of the design features of the bioprosthetic valve, that could be introduced once the ability to deliver a valve had been confirmed.
- The SATH program has been in existence for more than a decade. The Directors have always been mindful of the need to monitor progress elsewhere in the world in this rapidly changing scene and have taken note of significant developments and trends elsewhere. In view of this, some of SATH’s projects have been aimed at expanding the technology platform where considered appropriate. An underlying objective has been to develop a ‘universal’ TAVR, variations of which could be delivered transfemorally as well as transapically and with a variety of sizes, allowing for both bioprosthetic and polymer leaflets. In addition, a number of cardiovascular devices that are based on the non-occlusive balloon system have been developed.
- As a final point, it should be noted that SATH is a spin-out company from the University of Cape Town and has been fully supported financially from within South Africa. The laboratories within which SATH is located are named after the late Professor Christiaan Barnard, who carried out the world’s first human heart transplant in the adjacent Groote Schuur Hospital over 50 years ago, in 1967.
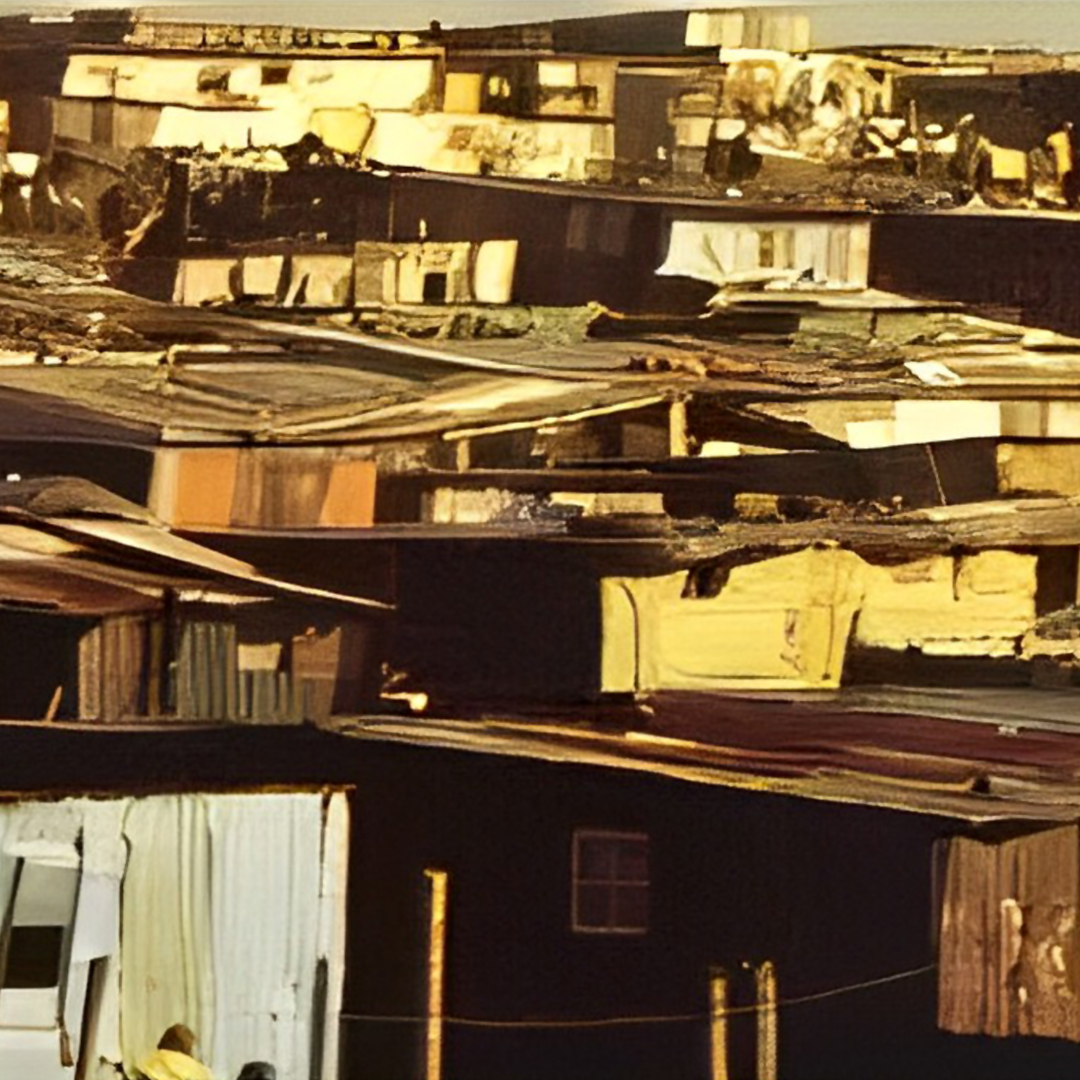
The Groote Schuur Hospital in Cape Town is where Professor Barnard carried out the world’s first human heart transplantation, and the current location of Strait Access Technologies.
Groote Schuur Hospital is a large, government-funded, teaching hospital situated on the slopes of Devil’s Peak in the city of Cape Town, South Africa. It was founded in 1938 and is famous for being the institution where the first human-to-human heart transplant took place, conducted by University of Cape Town-educated surgeon Christiaan Barnard on the patient Louis Washkansky.
